A team of international scientists has recently identified a distinct set of proinflammatory mediators and metabolites associated with the fatal consequences of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Moreover, they have established a link between gut microbiome alteration and hyper-inflammatory response in patients with severe COVID-19. The study is currently available on the bioRxiv* preprint server.
Background
Aberrant activation of interferon signaling together with excessive production of proinflammatory mediators is the major determinant of coronavirus disease 2019 (COVID-19) severity. Moreover, SARS-CoV-2-induced metabolic reprogramming further contributes to this hyperinflammatory state, leading to disruption of host cell homeostasis and progression of infection.
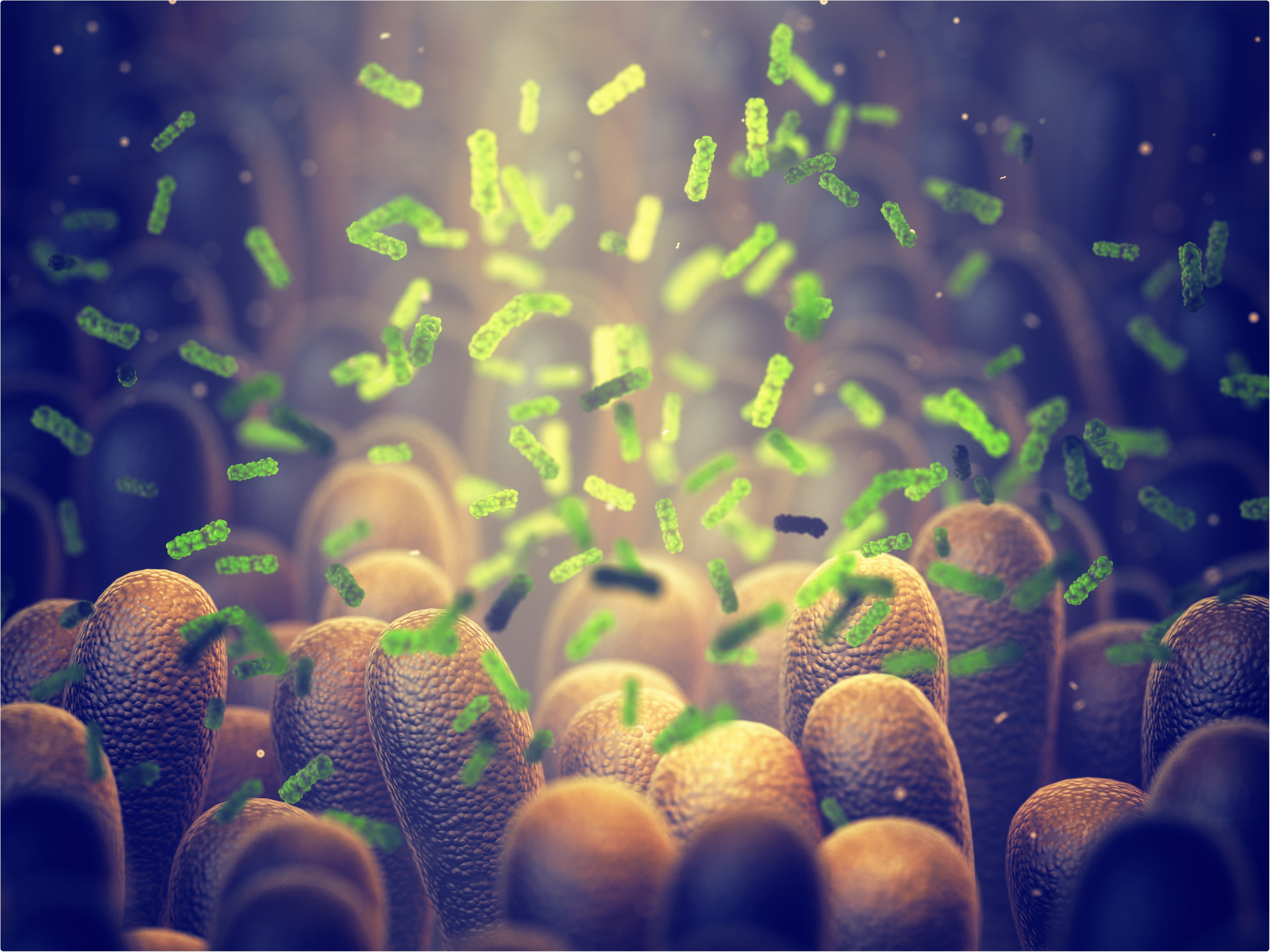
The diverse communities of beneficial microorganisms present in the human gastrointestinal (GI) tract play essential roles in regulating metabolic and immune functions in cells. In addition, immunoregulatory microbial metabolites can trigger a range of signaling pathways in host cells to protect against harmful pathogens.
In the current study, the scientists have aimed to identify distinct metabolic and immune markers that can predict the severity of SARS-CoV-2 infection.
They conducted multi-omics analyses on hospitalized COVID-19 patients to identify the patterns of immune-metabolic-microbial interactions associated with mild/moderate, severe, and fatal COVID-19.
Immunological and metabolic markers associated with disease severity
The scientists measured the blood levels of 54 immune mediators in hospitalized COVID-19 patients with varying severities. Of these mediators, 28 showed significantly different levels between patients with mild/moderate or severe disease. Moreover, they observed a significant variation in the levels of eight immune mediators between severely ill COVID-19 patients who eventually survived or died. These mediators were soluble intercellular adhesion molecule-1, monocyte chemoattractant protein-1, interleukin (IL)-8, macrophage-derived chemokine, interferon gamma-induced protein-10, IL-15, IL-1 antagonist, and thymic stromal lymphopoietin.
In a separate set of experiments, they measured the blood levels of metabolites in hospitalized COVID-19 patients with varying severities. They observed a significant variation in the levels of 140 metabolites between severely ill patients who eventually survived or died. Compared to healthy participants, mildly and severely affected patients showed substantial differences in the levels of 377 and 583 metabolites, respectively.
Specifically, metabolites associated with tryptophan, polyamine, histidine, lipid, bile acid, and antioxidant metabolic pathways showed the highest variations between patients with varying severities. Regarding the gut microbiome, significantly altered levels of microbial metabolites were observed in patients with severe or fatal disease.
.jpg)
Gut microbiome and COVID-19 severity
The scientists analyzed the diversity and composition of the gut microbiome using fecal samples of hospitalized COVID-19 patients. They observed significant differences in microbiome beta diversity among patients with varying disease severities. However, they did not observe any such difference for alpha diversity. They identified two distinct microbiome clusters, with one associated with severe and fatal disease and the other one associated with mild or moderate disease.
By analyzing genus-level composition, they observed that the high-risk microbiome cluster exhibits higher levels of harmful microbes and lower levels of anti-inflammatory, protective microbes. Furthermore, these changes in microbiome characteristics were significantly associated with changes in blood levels of immune mediators.
Immune mediator – metabolite – microbiome interactions
The scientists conducted weighted gene correlation network analysis on a number of immune mediators, metabolites, and microbial genera. They identified five modules that were significantly associated with different disease outcomes.
The module that showed a significant positive association with disease severity and mortality contained the majority of severe COVID-19-related cytokines, metabolites, and microbial genera together with coagulation-linked fibrinopeptides and tryptophan metabolism products.
In contrast, four modules that showed a significant negative association with disease severity and mortality contained anti-inflammatory and beneficial microbes together with short-chain fatty acids and IL-17A.
.jpg)
Study significance
The study identifies a distinct set of 8 circulating cytokines and 140 circulating metabolites that can increase mortality risk in severely ill COVID-19 patients. Moreover, the study reveals that elevated levels of harmful gut-microbes and reduced levels of beneficial microbes are associated with a poor prognosis of COVID-19.
.jpg)
As mentioned by the scientists, these biomarkers can be used clinically to identify high-risk individuals and further explore the relationship between the gut microbiome and inflammation in the context of SARS-CoV-2 infection.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Source
"severe" - Google News
November 01, 2021 at 12:39PM
https://ift.tt/3nNkZH7
Alteration in gut microbiome may lead to hyperinflammation in severe COVID-19 - News-Medical.Net
"severe" - Google News
https://ift.tt/2OrY17E
Shoes Man Tutorial
Pos News Update
Meme Update
Korean Entertainment News
Japan News Update
Bagikan Berita Ini















0 Response to "Alteration in gut microbiome may lead to hyperinflammation in severe COVID-19 - News-Medical.Net"
Post a Comment